About Cervical Radiculopathy
Cervical radiculopathy is the clinical description of when a nerve root in the cervical spine becomes inflamed or damaged, resulting in a change in neurological function. Neurological deficits, such as numbness, altered reflexes, or weakness, may radiate anywhere from the neck into the shoulder, arm, hand, or fingers. Pins-and-needles tingling and/or pain, which can range from achy to shock-like or burning, may also radiate down into the arm and/or hand.
About Cervical Radiculopathy
Cervical radiculopathy is the clinical description of when a nerve root in the cervical spine becomes inflamed or damaged, resulting in a change in neurological function. Neurological deficits, such as numbness, altered reflexes, or weakness, may radiate anywhere from the neck into the shoulder, arm, hand, or fingers. Pins-and-needles tingling and/or pain, which can range from achy to shock-like or burning, may also radiate down into the arm and/or hand.
How Cervical Radiculopathy Develops
Cervical radiculopathy is a rare condition that occurs slightly more often in men than women. 2 It is more likely to occur in older people due to spinal degeneration, with some estimates putting the highest risk for ages 50 to 54. When cervical radiculopathy occurs in younger people, it is more likely due to disc herniation or injury.
Cervical radiculopathy signs and symptoms most commonly appear intermittently at first—coming and going—but they could also develop suddenly or gradually. Some movements or head positions, such as putting the neck in extension (with the head back), may exacerbate the symptoms in some cases.
Most cases of cervical radiculopathy are self-limiting and go away on their own. There is limited evidence for whether any one nonsurgical treatment is more effective than others. 3 In the early stages, most recommendations are to try a combination of one or more treatments, such as rest or activity modification, physical therapy, manual manipulation, ice and/or heat therapy.
The two most common causes of cervical radiculopathy include:
Cervical Foraminal Stenosis
When a foramen (bony opening where a nerve root exits the spinal canal) narrows and becomes smaller, the nerve root has less space and may become impinged. Degenerative changes related to cervical osteoarthritis and/or cervical degenerative disc disease may result in nearby bone spurs (osteophytes), thickening ligaments, or a bulging disc that pushes against the nerve root in the foramen. Cervical foraminal stenosis is the most common cause of cervical radiculopathy.
Cervical Herniated Disc
If the inner material of the cervical disc leaks out and inflames or impinges the adjacent nerve, it can cause cervical radiculopathy. A herniated disc is more likely to occur from an injury or strenuous activity, which may explain why it is the most common cause of cervical radiculopathy in younger people (20s or 30s).

The two most common causes of cervical radiculopathy include:
Cervical Foraminal Stenosis
When a foramen (bony opening where a nerve root exits the spinal canal) narrows and becomes smaller, the nerve root has less space and may become impinged. Degenerative changes related to cervical osteoarthritis and/or cervical degenerative disc disease may result in nearby bone spurs (osteophytes), thickening ligaments, or a bulging disc that pushes against the nerve root in the foramen. Cervical foraminal stenosis is the most common cause of cervical radiculopathy.
Cervical Herniated Disc
If the inner material of the cervical disc leaks out and inflames or impinges the adjacent nerve, it can cause cervical radiculopathy. A herniated disc is more likely to occur from an injury or strenuous activity, which may explain why it is the most common cause of cervical radiculopathy in younger people (20s or 30s).
Other Causes of Cervical Radiculopathy
While much less common, other potential causes of cervical radiculopathy include:
Fracture. If part of a vertebra becomes fractured, the resulting instability or foraminal narrowing in the cervical spine may impinge a nerve root. Such a fracture could be caused by an injury or cervical spondylolisthesis (where one vertebra slips in front of another).
Tumor. A tumor, whether malignant or benign, may grow nearby and push against a nerve root.
Infection. Various spinal infections and—less commonly—systemic infections can lead to inflammation and/or damage to a nerve root.
Sarcoidosis. A rare disease that can cause granulomas (lumps) to grow on any organ in the body.
Other conditions may also compress or cause damage to the cervical nerve root. It is also possible for a congenital anomaly to result in a narrowed foramen or other changes that increase the likelihood for cervical radiculopathy to develop.
Cervical Radiculopathy Symptoms
Neurological Deficits in Cervical Radiculopathy
Cervical radiculopathy involves one or more of the following neurological deficits that may be experienced in the neck, shoulder, arm, hand, and/or fingers:
Sensory. Feelings of numbness or reduced sensation in the skin. There may also be tingling, electrical sensations.
Motor. Weakness or reduced coordination in one or more muscles.
Reflex. Changes in the body’s involuntary (automatic) reflex responses. Some examples may include diminished ability to respond when the skin touches hot or cold, or possibly a reduced triceps or biceps reflex when the elbow is tapped by a rubber hammer during an exam.
Cervical nerve roots are comprised of both motor and sensory fibers. Whether cervical radiculopathy signs involve diminished motor movement or sensation (or both) depends on which fibers are damaged by the radiculopathy.
How Pain May Feel with Cervical Radiculopathy
Cervical radiculopathy is typically accompanied by some form of radicular pain, but not always. In cases where cervical radiculopathy involves pain, it can range anywhere from a dull, general discomfort or achiness to a sharp, shock-like or burning pain.Cervical radicular pain may be felt anywhere from neck all the way down the arm into the fingers.
While a radiculopathy is commonly accompanied by radicular pain, the two are not the same. A radiculopathy involves a neurological deficit, whereas radicular pain can occur without a neurological deficit. It is possible to have cervical radiculopathy with little to no pain in the neck and/or arm, but most cases do involve pain in addition to the neurological deficits.
Cervical Radiculopathy Signs and Symptoms by Location
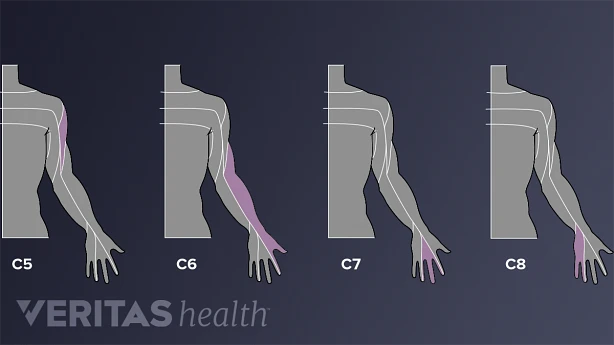
Cervical radiculopathy signs and symptoms differ depending on which nerve root is affected. For example, C6 radiculopathy occurs when the nerve root that runs above the C6 vertebra is affected.
While any patient’s specific signs and symptoms can vary widely and do not always follow a predictable pattern, 1 the following are common descriptions for how cervical radiculopathy may differ by location:
C5 radiculopathy. Tingling, numbness, and/or pain may go from the neck into the shoulder and/or down the arm and into the thumb. Weakness may be experienced in the shoulder or upper arm.
C6 radiculopathy. Tingling, numbness, and/or pain may radiate through the arm and into the second digit (index finger). Weakness may occur in the front of the upper arm (biceps) or wrist.
C7 radiculopathy. Tingling, numbness, and/or pain may be felt down the arm and into the middle finger. Weakness may be experienced in the back of the upper arm (triceps).
C8 radiculopathy. Tingling, numbness, and/or pain may radiate down the arm and into the little finger. Handgrip strength may be reduced.
See All About the C7-T1 Spinal Segment (Cervicothoracic Junction)
Less commonly, cervical radiculopathy can occur higher in the cervical spine, such as C4 radiculopathy or higher. While rare, it is also possible to have nerve compression or inflammation at multiple levels of the cervical spine at the same time, resulting in multiple radiculopathies.

Diagnosis of Cervical Radiculopathy
The process of diagnosing cervical radiculopathy typically involves a physical examination and review of the patient history. For cases that are more complicated or severe, and for the confirmation of the exact etiology of the symptoms, imaging studies and other advanced diagnostics may be needed.
Patient History and Physical Exam
When a person presents with suspected cervical radiculopathy, such as pins-and-needles tingling, weakness, or numbness in the shoulder, arm, and/or hand, the doctor will likely start with the following:
Patient history
Information is gathered regarding current signs and symptoms, any prior or current illnesses or conditions, accidents or injuries, family history, and lifestyle. This medical background can help give a better picture of what might need further investigation.
Physical exam
The neck is palpated (felt) for any abnormalities or tenderness. The arm and hand are tested for any reductions in strength, sensation, or reflexes. Head and neck range of motion are also checked.
Spurling’s test
As part of the physical exam, Spurling’s test enables the doctor to see if compressing the cervical spine can reproduce or (temporarily) worsen the patient’s radicular symptoms. This test is typically done by having the patient bend the head to the side where symptoms have occurred, and then the doctor gently applies pressure to the top of the head. This process will cause the cervical foramen—bony openings in the spine where nerve roots exit—to compress and narrow, which might have the effect of compressing a nerve root and reproducing the radicular symptoms that the patient has been experiencing. If Spurling’s test reproduces the patient’s radicular symptoms, cervical radiculopathy is likely present. Although, it is common for cervical radiculopathy to still be present even if Spurling’s test does not reproduce the symptoms.
Patients who are already showing signs of cervical myelopathy (compression of the spinal cord) or started having radicular symptoms after a traumatic injury (and thus might have a fracture) should not be given Spurling’s test.
A positive Spurling’s test is usually enough to safely start a nonsurgical treatment program for cervical radiculopathy.
Advanced Diagnostic Techniques
In some cases, especially if signs and symptoms have not been subsiding with conservative treatment, advanced diagnostic techniques might be requested, such as:
Imaging studies
Imaging of the body may show how a cervical herniated disc or bone spur is impeding a nerve root in the neck. Magnetic resonance imaging (MRI) is the most common imaging study used when checking for cervical radiculopathy because it shows nerves and other soft tissues, such as herniated discs, so clearly. For people who cannot have an MRI for medical reasons, or if a better image of the bones is needed, an x-ray or CT scan may be advised.
Electrodiagnostic testing
These types of tests check how nerves are functioning. Two components of electrodiagnostic tests include:
Electromyography (EMG), which can check nerve and muscle function as well as nerve communication with muscle fibers by monitoring electrical activity in the muscle
See Electromyography (EMG)
Nerve conduction studies (NCS), which check whether nerves are sending signals at an appropriate speed
Imaging studies can be expensive, and electrodiagnostic testing can be uncomfortable. So these diagnostic methods tend to only be used if needed to help reach a diagnosis.
About Physical Therapy
![dr ronjon paul md (1020x681px) - how is [condition] diagnosed? https://paulspine.com/wp-content/uploads/2021/01/dr-ronjon-paul-md-1020x681px-how-is-condition-diagnosed.jpg](https://paulspine.com/wp-content/uploads/2021/01/Dr-Ronjon-Paul-MD-1020x681px-How-is-condition-diagnosed.jpg)
How is Acute Neck Pain diagnosed?
The diagnostic modality of choice is x-ray imaging to give the physician a full view of the back and neck structures, though in many cases imaging is not even required. A doctor can usually make the diagnosis with only the physical examination and patient history, but in some cases further diagnostics will be ordered to exclude more concerning possibilities. The primary goal of treatment for acute neck pain is to resolve the episode as quickly as possible and return the patient to prior functioning.